INTRODUCTION
Phoneutrism caused by Phoneutria spiders (commonly known as Brazilian wandering spider or banana spider) is one of the most important clinical syndromes resulting from bites of these spiders in Brazil1,2,3,4,5. They are habitually nocturnal and found in banana plants, palm trees, and bromeliads6. Phoneutria spp. are also usually found in shoes, log piles, among discharged matter, and construction materials as well as in banana bundles, which explain the greater frequency of bites in feet and hands7. According to the Brazilian Notifiable Diseases Surveillance System (Sistema de Informação de Agravos de Notificação - Sinan), from 2013 to 2016, 11,860 accidents caused by Phoneutria species were recorded8.
The venom of Phoneutria is composed by a high diversity of proteins and peptides, including neurotoxins which act on plasma membrane ion channels and chemical receptors of the neuromuscular control systems of the victim9. The venom can cause depolarization of myofibers and nerve endings at the myoneural junction, activation of the visceral efferent nervous system, causing the circulation of adrenergic neurotransmitters and acetylcholine8,10,11.
In Brazil, the most studied venom of wandering spider species belongs to Phoneutria nigriventer12. P. nigriventer venom activates and delays the inactivation of neuronal Na+ channels13,14. The composition of peptides in the venom of P. nigriventer can generate contractures on vascular smooth muscle and can also upsurge capillary permeability by triggering the tissue kallikrein system and stimulating the discharge of nitric oxide15,16,17,18,19. It was also showed that the venom lags gastric emptying in rats, in part by the venom-induced catecholamine discharge20.
Accidents by Phoneutria species cause local pain that may radiate, edema, erythema, paresthesia (burning, numbness, itching), sweating near the site of the bite, hypothermia, tachypnea, bradypnea, blurred vision, pallor, cyanosis, prostarion, generalized muscle fasciculation (involuntary muscle contraction), vomiting, cardiac arrhythmia, tachycardia, poor peripheral perfusion, elevated blood pressure, and, depending on severity, may progress to death7,8,21,22,23,24. In many cases, the victim may not notice the bite or chooses not to seek treatment through negligence or difficulties of access to health care facilities.
A clinical epidemiological study including 422 cases of patients from 1984 to 1996 (age ranging from 9 months to 99 years old) bitten by Phoneutria showed that most patients presented only local complaints, mainly pain and edema7. Most of the patients (89.8%) presented mild symptoms, 8.5% presented moderate envenomation, and only 0.5% had severe envenomation which was only confirmed in children. In few patients (1.2%) symptoms of intoxication were not reported. Some of the unusual or acute systemic manifestations, reported so far in the literature, were toxin-induced priapism and acute pulmonary edema followed by death7,25.
Despite of the medical importance of Phoneutria, there are very few detailed clinico-epidemiological diagnosis and descriptions of systemic envenoming21, and, because of reporting failures, there is a gap in epidemiological data. Informations about clinical manifestations in severe cases are unusual, therefore atypical manifestations needs to be reported with precision. Here, the case of an accident caused by the banana spider Phoneutria reidyi with Raynaud phenomenon sequela is reported. All photographs and case information are included with written consent from the patient.
CASE REPORT
A healthy 23 years old female was bitten on middle toe of the left foot (Figures 1A, 1C; Figure 2A). The victim was in a small ranch near Manaus, Amazonas State, Brazil. The spider was identified as a female Phoneutria reidyi (F. O. Pickard-Cambridge, 1897).
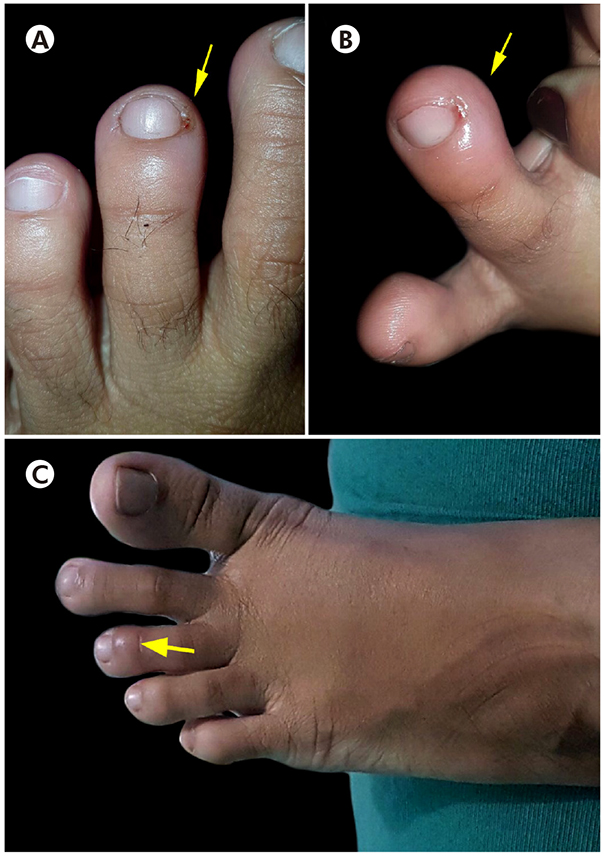
Photos: Lidianne Salvatierra.
A: Fang marks on middle toe of left foot; B: Edema; C: Two months after bite.
Figure 1 - Phoneutria reidyi bitten on middle toe of the left foot of a victim from Manaus, Amazonas State, Brazil
Initially, the spider bite caused a local redness on middle toe, but no significant lesion, erythema or other visible effects developed. Later, the middle toe became swollen, painful, and with local skin discoloration (Figure 1B). During the next few days, the patient experienced mild pain and paresthesia in the middle toe, but did not seek medical advice. In the following days, the toe turned darker (cyanosis). The pain, swelling, and cold sensation on the toe area persisted for several days along with numbness and desquamation around the bite site (Figure 2B). Just after one month from the accident, the victim went to the hospital complaining about the persistent pain, discoloration, and cold sensation on toe. The patient informed the attending physician about the spider bite.
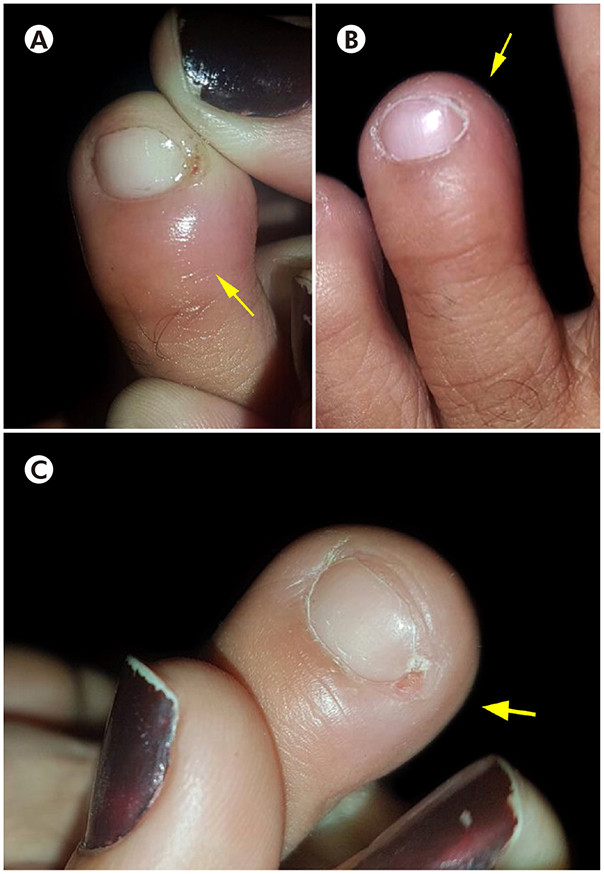
Photos: Lidianne Salvatierra.
A: Fang marks and edema; B: Desquamation around the bite site; C: Middle toe after four months of bite.
Figure 2 - Middle toe in the left foot of wandering spider victim from Manaus, Amazonas State, Brazil
A blood test was ordered to check blood sugar and other infections. The laboratory findings were: white blood cell count of 808×10/mm3 (lymphocytes 35.9%, monocytes 8.3%, granulocytes 0.2%), red blood cell count of 4.79×106/mm3, hemoglobin 13.1 g/dL, platelet 375×103/mm3, hematocrit value of 39.6%, glucose level of 87.4 mg/dL, creatinine value of 0.63 mg/dL, mean corpuscular volume (MCV) of 82.7 fL, mean corpuscular hemoglobin (MCH) of 27.3 pg, mean corpuscular hemoglobin concentration (MCHC) of 33.1%, red cell distribution width (RDW- SD) of 42 fL, and red cell distribution width (RDW- CV) of 14.1%. The blood film was essentially within normal limits.
The clinical examination indicated poor circulation on middle toe. The reduced blood flow was the cause of pain, cold sensation, and pale blue coloration on toe. In order to detect a possible clot or reflux, an aortography, extremity arteriography, venous and arterial duplex vascular ultrasound scan of the lower extremities were carried out and all results were normal. Finally, x-ray exam of left leg was performed to detect the cause of pain and swelling and the result was also normal. The exams were performed to rule out the possibility of venous and arterial thrombosis due to the use of oral contraceptives by the patient.
During all this period, the patient received no anti spider venom therapy nor other supportive or symptomatic treatment. The patient applied pequi oil (Caryocar brasiliense) on the bite site following a non-medical advice, and used acetaminophen to relieve pain. The patient experienced persistent pain for eight months, which also radiated to plantar area, and persistent abnormal blood flow (Raynaud phenomenon) as sequelae. After ten months from the accident, the patient followup showed that the wound healed (Figure 2C) and the unusual symptoms ceased without tissue damage.
DISCUSSION
Phoneutrism systemic manifestations are uncommon, although in severe cases may include arterial hypertension, priapism, and pulmonary edema7,21. In this reported case, the signs and symptoms that were developed included pain, edema, poor peripheral perfusion, and paresthesia. The radiated pain and edema observed in the present case are the two most frequent symptoms and emerge from either secondary ischemia to vasospasm or break of myelin wrapping on myofibers. These findings are similar to the previously reported cases of phoneurism1,2,11,21,22. However, Raynaud phenomenon, characterized here as persistent low circulation and peripheral neuropathy, has never been reported in the literature as a long-term phoneutrism sequelae.
Raynaud phenomenon is a recurrent vasospasm characterized as the constriction of the small blood vessel (arteries or arterioles) of the extremities that results in occasional changes in skin color of the area, such as pallor, cyanosis or both26. The development of Raynaud phenomenon occurs by interactions among nerve fiber endings, smooth myofibers, and endothelium that is induced by soluble mediators settings and is influenced by the patient’s surrounding environment27, such as venomous animal bites. Raynaud phenomenon may be correlated with and can be the initial symptom of various conditions or disorders, both local and systemic28.
The symptoms are usually entirely reversible, painless, and typically do not progress to tissue injury. However, it has been documented that some poisonous species of snakes29,30 and fish31 can cause Raynaud phenomenon. Sathyanathan and Mathew29 reported Raynaud phenomenon and gangrene in the opposite limb due snakebite intoxication; and Kularatne and Ratnatunga30 described severe Raynaud's syndrome leading to escalating gangrene of distal extremities, and adult respiratory distress syndrome, along with the noted aggravations of acute renal cortical necrosis and haemostatic impairment.
Multiple mechanisms have been suggested for Raynaud phenomenon following venomous animal bites, which the most common include plain toxic response on the muscular tissue of the heart and coagulation disorders, or arterial spasm leading to vasoconstriction induced by some snake venom hemorrhagins or endothelins, for instance32.
To the best of our awareness, this is the prime address of a Phoneutria spider accident with Raynaud phenomenon as a sequela. The vasospasm observed in this case evolved to a benign reversible Raynaud phenomenon, but did not lead to tissue damage. Collectively, the present clinical case and those of similar and earlier unusual reports show that venomous animal injuries can cause clinical symptoms that range from patient to patient depending on the physiological response to the venom, given that more sensitive individuals can develop deeper reactions. Some factors, as bite site and underlying health problems, may account for this variability in the severity of clinical signs. Also, it is likely that immediate and adequate medical care diminishes the severity of the manifestation and promotes positive results.
In case of accidents, several symptoms of poisoning have been observed, and if the symptoms are not quickly treated, they can evolve to sequelae or even progress to death. Hence, the rigorous identification of the venomous specimens and the lithe clinical care provided to the patient can significantly reduce morbidity and mortality as well as can avoid sequelae.
CONCLUSION
Accidents with venomous animals are considered a neglected public health issue, and spider bites are especially frequent. The outcomes of spider bites are largely benign but complications can occur. Patients with a suspicion of impending and unusual symptoms should be closely monitored, since they may need more medical attention. Efficient evaluation and inspection and early specific treatment are the main guidance to manage severe cases of intoxication by venomous animals. The present study brings light to sequelae of phoneutrism rarely reported in literature. Further and careful documentation of verified cases, such as this one reported here, will reinforce the medical significance of Brazilian wandering spider bites.









 text in
text in 


