INTRODUCTION
Death is a natural process of human development and is present in the daily life of health professionals. Despite this, modern Western culture avoids discussing death-related issues1, and health progress has led to treatments that can postpone death2,3. In Intensive Care Units (ICU), this progress has led to the maintenance of life, sometimes beyond ethical boundaries4,5. A battle against death at all costs is established1, generating problems in the acceptance of human finitude and the limitations to therapeutic healing. Rather than guaranteeing a "good death"6,7, health professionals try to avoid loss of life, even for patients out of therapeutic possibilities (POTP). The concept of "good death" is complex8,9, because it means that POTP, their families, and caregivers can be free from pain, distress, and suffering, and patients are dying comfortably, following patients' wishes, beyond clinical, cultural, and ethical patterns8,9,10. Consequently, ICU professionals, like nurses and physicians11,12, find difficulty in dealing with death and experience sensations of sadness, helplessness, loss, failure, fear, guilt, and denial.
This subject appears to be insufficiently discussed during health professionals' training13,14,15. Health workers seem to be far removed from the socio-anthropological dimensions of death12, and quality of life is often no longer the goal. This shift in goals underlines the need for reflection on the meaning of death and the professionals' attitudes facing a POTP16,17. One systematic review18 showed that, in general, death is represented in different ways among students and nursing staff. The end of life is conceived as a transition, passage to heaven, separation, loss, pain, unknown, relief, and duty accomplished, as a natural process related to the development of the human being, or simply as an end. Other studies have been developed on this subject19,20,21,22,23. However, only one study with ICU workers in hospitals located in the Brazilian Legal Amazon was identified, but it was specific to the death of children, and using a qualitative approach24.
In Brazil, the new Code of Medical Ethics, which guides terminal illness situations, has incorporated some suggestions from the medical profession and civil society on palliative care for terminally ill patients25, in which removing or limiting life support for patients in the end-of-life (orthothanasia) is one of these recommendations. On the other hand, the Nursing Ethics Code declares that it is prohibited to promote or participate in a practice aimed at anticipating the death of the person26, so these codes still lack a full understanding of society25,27. Discussion is needed, even among health professionals, commonly exposed to conflicts inherent to the theme of death, particularly in the ICU setting, and especially after the COVID-19 pandemic, which made death even more evident28,29,30,31,32. In other countries, teaching ethics codes in the nursing curriculum for students and continuous education for staff is also purposed33,34,35.
We hypothesized that the perceptions/feelings regarding death in the ICU environment for most health professionals have not yet incorporated the concept of "good death", and that their perceptions and attitudes would be determined by demographic and sociocultural characteristics. Avoiding death is a goal, even in the case of POTP. This study aimed to describe the perceptions, feelings, and attitudes of these professionals facing ICU patients' death, as well as to analyze demographic and sociocultural factors associated with these outcomes.
MATERIALS AND METHODS
ETHICAL APPROVAL
The study was prepared following the principles of Resolution No. 466, from December 12, 2012, and complementary to the Brazilian National Health Council. The confidentiality of the participants' records was ensured. For the database organization, an identification number was adopted to de-identify the participants, guaranteeing their anonymity. The research was approved on February 25th, 2010, by the Research Ethics Committee (No. 006168/2009-70) of the Presidente Dutra University Hospital, from Maranhão Federal University (HUUFMA). All participants signed an Informed Consent Form, with participation in the study being voluntary, anonymous, and confidential.
STUDY DESIGN AND SETTING
This study is part of one broader research with a qualitative-quantitative approach, in which some qualitative results were previously presented20. In this article, we present a cross-sectional investigation, using quantitative data from a survey conducted with nurses and physicians of the four
ICUs from HUUFMA, at São Luís city, Maranhão State, one of the nine states belonging to the Brazilian Legal Amazon. This is the biggest and most important teaching hospital in the state linked to the Brazilian Public Health System (Sistema Único de Saúde - SUS), that contains general diseases (12 beds), cardiology (eight beds), neonatal (20 beds), and pediatric (nine beds) ICUs. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement36.
PARTICIPANTS
We intentionally sampled HUUFMA among the hospitals of the city. The research was addressed for all nurses and physicians in the Hospital (non-random sampling). Of the 118 professionals (62 nurses and 56 physicians) working in the ICU of HUUFMA, 13 (10 nurses and three physicians) were not included due to their refusal to answer the questionnaire, seven (three nurses and four physicians) for incomplete questionnaires, and one physician, because he was responsible for the research, reaching 97 (93.2%) of valid questionnaires.
Nurses and physicians were chosen because they represent the health categories that have a broader engagement with the patients and families through providing therapeutic care, performing procedures, providing information, and communicating bad news.
DATA SOURCE, DATA COLLECTION, AND VARIABLES
A self-administered structured questionnaire was used as data collection instrument. The questionnaire was given to each employee at the beginning of his/her shift in the ICU and collected at the end. It consisted of 44 questions divided into sections (Table 1). The steps used to determine the questionnaire reliability and validity were: face and content validity, and test-retest reliability. For this validation, a team of experts was consulted.
Table 1 - Description of study variables, with respective sections (blocks in the theoretical model) and categories (response options)
| Sections | Variables | Categories |
|---|---|---|
| Demographic | Sex | Male or female |
| Age | In years | |
| Sociocultural | Marital status | Has a partner (married or in a consensual union) or not (single, separated/divorced or widowed) |
| Do you have a religion? | Yes or no | |
| Give importance to religion | Yes or no | |
| Personal experience with death | When was your first personal experience with death | In childhood, adolescence, or adulthood |
| Professional qualifications and professional experiences with the patient's death | Professional category | Physician or nurse |
| Time since graduation | The time between graduation and the interview date (categorized according to tertiles distribution in ≤ 10 years, 11-15 years, and > 15 years) | |
| ICU specialty | General, cardiologic, or infant (neonatal and pediatric) | |
| How long work in ICU | Categorized according to the median in ≤ 7 years, and > 7 years | |
| Hours working in ICU | Categorized according to the median distribution: ≤ 40 hours/week or > 40 hours/week | |
| Discussion of the subject at graduation | Yes or no | |
| Discussion of the topic of death in postgraduation | Yes or no | |
| Discussion of the subject in professional life | Yes or no | |
| Patients' age of the first professional death experience | In childhood, adolescence, or adulthood | |
| The main memory of the first experience with a patient's death | Giving news to the family, family reaction, caring for the body, or other | |
| Perceptions/ feelings about the death of a patient in the ICU | Meaning of death (outcome 1) | Beginning/freedom, failure/guilt, or other |
| Meaning of death in the terminal patient (outcome 2) | Relief/rest for the patient or I feel pain (pain for the professional) | |
| Attitudes toward the death of a patient in the ICU | To take responsibility for giving the news of the death (outcome 3) | To share responsibility with the team, to take responsibility alone, or to run away |
| To reanimate the patient out of therapeutic possibilities (outcome 4) | Agree or disagree | |
| To discuss do-not-resuscitate orders with the family (outcome 5) | Agree or disagree |
ICU: Intensive Care Unit.
BIAS
Data were entered in the Microsoft Excel® program by two independent typists, and these were later compared to control possible typing errors to reduce bias. Besides, data collection was performed by a single previously trained interviewer.
DATA ANALYSIS
The statistical analysis was performed using STATA® v14.0 (Stata Corp., College Station, TX, USA). Discrete or continuous variables were summarized as the mean ± standard deviation (SD) and categorical or ordinal variables as absolute (n) and percentage (%) values. The chi-square and Kruskal-Wallis tests were used to evaluate differences in data distribution within the categories of response variables (outcomes).
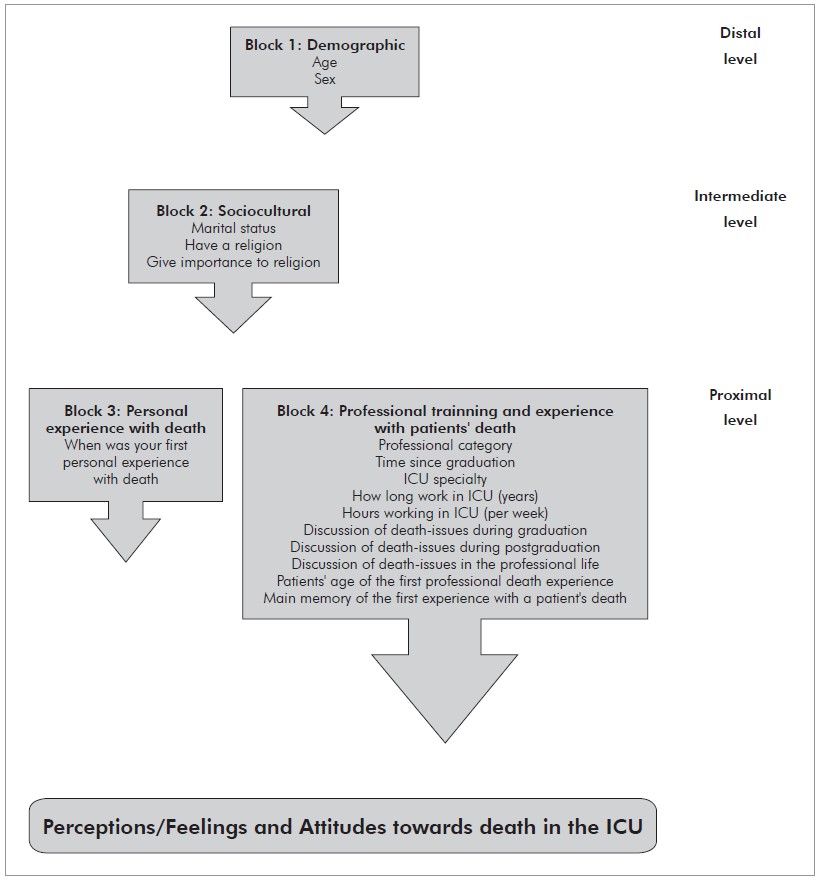
Associations among the explanatory variables and outcomes were estimated using the odds ratio (OR) and the respective unadjusted and adjusted 95% confidence intervals (95%CI). Five different outcomes were considered: meanings of death (model 1); meanings of the death in terminally ill patients (model 2); attitude towards giving news of death (model 3); resuscitation of a POTP (model 4); and discussion about do-not-resuscitate orders (model 5). Models 1 and 2 represent the professionals' 'perceptions/feelings' towards death, and models 3 to 5 represent their professional 'attitudes' when confronted with dying. The remaining (explanatory) variables were grouped into blocks for input into the regression analyses in a hierarchical approach specified in figure 1. Hierarchical modeling allows the differential treatment of variables by levels of determination on the outcome, therefore considering mediation and confounding adjustments37. The variables selected for the theoretical model and their distribution in the different levels of determination followed recommendations from the literature38,39,40, in which five models (according to different outcomes) were adjusted. In models 1 and 3, estimates were calculated using multinomial regression analysis and, for the other models, it was used logistic regression analysis.
Initially, univariate analyses were performed. In multivariate analyses, the variables from the distal level (block 1) were initially included in the model, keeping only those with a p-value < 0.10. Intermediate-level variables (block 2) were then included, ensuring those from the previous level and any variables from this level with p < 0.10. Proximal level variables (blocks 3-4) were then included, repeating the p-value criteria to keep variables. Thus, the associations were adjusted to variables from the same and previous levels, and the p < 0.10 was used to select variables for the adapted models, but p < 0.05 was considered to reject the null hypothesis.
RESULTS
The age of the respondents ranged from 24 to 62 (39.6 ± 7.6) years old, and the time since graduation ranged from 2 to 32 (14.3 ± 7.8) years. The length of service in the ICU ranged from 1 to 32 (9.9 ± 6.1) years (data not shown). Most of the participants were female (77.3%), aged less than 38 years old (53.6%), living without a partner (68.0%), and assuming a religion (92.8%), but not as an essential aspect in their lives (87.6%). The first personal experience with death was during childhood in 47.4% of the sample, and the professional experience was with a child/adolescent patient in 37.5% of the respondents. Most of the professionals interviewed were physicians (53.6%), practicing for more than 11 years (56.7%), specifically in ICUs over seven years (52.6%), and mainly in the children's ICU (54.6%). Not all professionals discussed the topic of death during graduation (49.5%), postgraduation (42.7%), and into the labor environment (62.9%). The first professional experience with death was mainly with a child/adolescent patient (37.5%), and their main memory of
this first experience with a patient's death was giving news to the family/family reaction (58.9%). Many workers interpreted the meaning of the death of an ICU patient as their failure/guilt (26.8%). However, if the patient was out of therapeutic possibilities, the predominant response was rest/relief (86.3%). Half of the nurses and physicians stated they share with the team the responsibility about the death's communication to the family. Most professionals (62.5%) disagreed according to the resuscitation of a POTP, and 66.7% agreed about discussing with the family the decision not resuscitating terminally ill patients (Table 2).
Table 2 - Characterization of ICU professionals from HUUFMA, São Luís, Maranhão State, Brazil, 2011-2012
| Variables | N | % | 95%CI |
|---|---|---|---|
| Block 1 - Demographic | |||
| Sex | |||
| Male | 22 | 22.7 | 14.3-31.0 |
| Female | 75 | 77.3 | 69.0-85.7 |
| Age (median) | |||
| ≤ 38 years old | 52 | 53.6 | 43.7-63.5 |
| > 38 years old | 45 | 46.4 | 36.5-56.3 |
| Block 2 - Sociocultural | |||
| Marital status | |||
| With partner | 31 | 32.0 | 22.7-41.2 |
| No partner | 66 | 68.0 | 58.8-77.3 |
| Do you have a religion? | |||
| Yes | 90 | 92.8 | 87.6-97.9 |
| No | 7 | 7.2 | 2.1-12.4 |
| Is religion important to you? | |||
| Yes | 12 | 12.4 | 5.8-18.9 |
| No | 85 | 87.6 | 81.1-94.2 |
| Block 3 - Personal experience with death | |||
| When was your first personal experience with death? | |||
| In childhood | 46 | 47.4 | 37.5-57.4 |
| In adolescence | 21 | 21.7 | 13.5-29.8 |
| In adulthood | 30 | 30.9 | 21.7-40.1 |
| Block 4 - Professional training and experience with patients' death | |||
| Professional category | |||
| Physician | 52 | 53.6 | 43.7-63.5 |
| Nurse | 45 | 46.4 | 36.5-56.3 |
| Time since graduation | |||
| ≤ 11 years | 42 | 43.3 | 33.4-53.2 |
| > 11 years | 55 | 56.7 | 46.8-66.6 |
| ICU specialty | |||
| General | 26 | 26.8 | 18.0-35.6 |
| Cardiological | 18 | 18.6 | 10.8-26.3 |
| Infant | 53 | 54.6 | 44.7-64.5 |
| How long work in ICUs? | |||
| ≤ 7 years | 46 | 47.4 | 37.5-57.4 |
| > 7 years | 51 | 52.6 | 46.2-62.5 |
| Hours working in ICU | |||
| ≤ 40 hours/week | 62 | 63.9 | 54.4-73.5 |
| > 40 hours/week | 35 | 36.1 | 26.5-45.6 |
| Discussion of death issues during graduation | |||
| Yes | 48 | 49.5 | 39.5-59.4 |
| No | 49 | 50.5 | 40.6-60.5 |
| Discussion of death issues during postgraduation | |||
| Yes | 41 | 42.7 | 32.8-52.6 |
| No | 55 | 57.3 | 47.4-67.2 |
| No information | 1 | -- | -- |
| Discussion of death issues in the professional life | |||
| Yes | 61 | 62.9 | 53.3-72.5 |
| No | 36 | 37.1 | 27.5-46.7 |
| The first professional experience with death was with: | |||
| A child/adolescent patient | 36 | 37.5 | 27.8-47.2 |
| An adult patient | 34 | 35.4 | 25.8-45.0 |
| An elderly patient | 26 | 27.1 | 18.2-36.0 |
| No information | 1 | -- | -- |
| The main memory of the first experience with a patient's death was: | |||
| Giving news to the family / Family reaction | 56 | 58.9 | 49.1-68.8 |
| Caring for the body | 7 | 7.4 | 2.1-12.6 |
| Other | 32 | 33.7 | 27.1-46.5 |
| No information | 2 | -- | -- |
| Outcomes | |||
| What is the meaning of death? (Outcome 1) | |||
| Start/Release for the patient | 15 | 15.5 | 8.3-22.7 |
| End of the patient's life | 17 | 17.5 | 10.0-25.1 |
| Failure/Guilt of the professional | 26 | 26.8 | 18.0-35.6 |
| Other | 39 | 40.1 | 30.4-50.0 |
| What is the meaning of the death of a terminally ill patient? (Outcome 2) | |||
| Rest/Relief for the patient | 82 | 86.3 | 79.4-93.2 |
| Pain for the professional | 13 | 13.7 | 6.8-20.6 |
| No information | 2 | -- | -- |
| Attitude toward death news (Outcome 3) | |||
| To share responsibility with the team | 48 | 50.0 | 40.0-60.0 |
| To assume responsibility alone | 27 | 28.1 | 19.1-37.1 |
| To run away | 21 | 21.9 | 13.6-30.1 |
| No information | 1 | -- | -- |
| Patients without therapeutic possibility should be revived (Outcome 4) | |||
| I agree | 36 | 37.5 | 27.8-47.2 |
| I disagree | 60 | 62.5 | 52.8-72.2 |
| No information | 1 | -- | -- |
| The order not to resuscitate should always be discussed with patient's family (Outcome 5) | |||
| I agree | 64 | 66.7 | 57.2-76.1 |
| I disagree | 32 | 33.3 | 23.9-42.8 |
| No information | 1 | -- | -- |
N: Frequecy; %: Percentual; 95%CI: 95% confidence interval; ICU: Intensive Care Unit; Dashes (--): Missing data.
The non-adjusted and adjusted analysis results are in tables 3 (the meaning of the death of an ICU patient) and 4 (professional attitudes). For model 1, in the adjusted analyses, having a personal experience with death in adulthood (OR = 6.5), being a physician (OR = 8.2), and working in the cardiology ICU (OR = 22.4) were associated with a higher chance of perceiving the patient died as a health worker failure/guilt instead of beginning/freedom for the patient. Those interviewed who had acted in the ICU for more time, presented a higher chance of interpreting death as an ending and not as a beginning/freedom (OR = 5.6). In model 2, the first personal experience with death during adolescence (OR = 6.5) and being a nurse (OR = 6.7) increased the chance of perceiving the death in a POTP as a painful experience for the professional and not as the patient rest/relief, after adjustment (Table 3).
Table 3 - Perceptions/feelings facing the death of ICU patients of health professionals from HUUFMA, São Luís, Maranhão State, Brazil, 2011-2012
| Variables | Model 1 (Meaning of death of an ICU patient) | Model 2 (Meaning of death in POTP) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-adjusted OR [95%CI] | Adjusted OR* [95%CI] | Non-adjusted OR [95%CI] | Adjusted OR† [95%CI] | ||||||||
| End | Failure/Guilt | Other | End | Failure/Guilt | Other | Pain | Pain | ||||
| First personal experience with death | |||||||||||
| Childhood | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | |||
| Adolescence | 1.2[0.2-6.8] | 1.7[0.3-10.0] | 0.5[0.1-2.3] | 1.2[0.2-6.8] | 1.7[0.3-10.0] | 0.5[0.1-2.3] | 6.5[1.1-37.2] | 6.5[1.1-37.2] | |||
| Adult age | 2.3[0.4-13.6] | 6.5[1.2-35.6] | 0.7[0.1-3.3] | 2.3[0.4-13.6] | 6.5[1.2-35.6] | 0.7[0.1-3.3] | 4.1[0.7-22.6] | 4.1[0.7-22.6] | |||
| Professional category | |||||||||||
| Nurse | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | 6.8[1.4-33.2] | 6.7[1.3-33.4] | |||
| Physician | 1.1[0.2-4.8] | 4.4[1.1-17.8] | 2.0[0.6-7.0] | 1.6[0.3-8.4] | 8.2[1.5-43.3] | 2.2[0.5-9.2] | Ref. | Ref. | |||
| ICU specialty | |||||||||||
| General | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | -- | -- | |||
| Cardiological | 4.0[0.3-49.6] | 8.0[0.7-90.0] | 2.8[0.2-30.9] | 8.8[0.5-152.1] | 22.4[1.3-392.1] | 5.9[0.4-89.2] | |||||
| Infant | 0.9[0.2-4.3] | 1.4[0.3-6.4] | 1.7[0.4-6.4] | 1.6[0.3-9.3] | 2.7[0.4-16.6] | 2.5[0.5-11.1] | |||||
| Time working in ICU | |||||||||||
| ≤ 7 years | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | -- | -- | |||
| > 7 years | 3.0[0.7-13.3] | 2.1[0.5-8.2] | 2.8[0.8-9.8] | 5.6[1.1-30.7] | 4.7[0.9-25.1] | 3.9[0.9-16.3] | |||||
OR: Odds ratio; 95%CI: 95% confidence interval; ICU: Intensive Care Unit; POTP: Patient out of therapeutic possibilities; Ref.: Reference category; Dashes (--): Not included in the multivariate model; Childhood: Neonatal and pediatric children. Only the variables with p-value < 0.05 in at least one of the models were kept. Model 1. Reference category: Beginning/Freedom. Model 2. Reference category: Rest/Relief. * In the adjusted model 1 entered the variables: Time of the first personal experience with death, professional category, type of ICU, time working in ICU, and load-time in the ICU; † In model 2 entered the variables: Time of the first personal experience with death and professional category.
In model 3, after adjustment, the graduation time around 11-15 years, compared to those who finished recently (OR = 5.0), and work in two or more ICUs (OR = 4.8) were associated with a higher chance to assume alone the responsibility of communicating the death to the family, rather than sharing it with the team. In model 4, physicians (OR = 1.2) have a higher chance of disagreeing to the resuscitation in a POTP compared with nurses. However, professionals who did not discuss the topic of death in their working environment (OR = 0.8) and those who had their first experience with death during the adult age (OR = 0.8) were more likely to agree with the resuscitation of a POTP, even after the model adjustment. In model 5, after setting, those workers who did not give central importance to religion presented a 20% more chance of agreeing with the resuscitation discussion with the patient's family (OR = 0.8) (Table 4). The coefficients about determination (R2) ranged from 11.8% to 17%, so the models variables explained a good percentage of oscillation in the results (data not shown). Factors such as professional's gender, age, and marital status were not associated with any of the study outcomes.
Table 4 - Health professional attitudes toward death in the ICU, São Luís, Maranhão State, Brazil, 2011-2012
| Variables | Model 3 (Attitude in the face of death news) | Model 4 (Resuscitation of the patient out of therapeutic possibilities) | Model 5 (Discussion of resuscitation with family) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-adjusted OR [95%CI] | Adjusted OR* [95%CI] | Non-adjusted OR [95%CI] | Adjusted OR† [95%CI] | Non-adjusted OR [95%CI] | Adjusted OR‡ [95%CI] | ||||||||
| To assume | To run away | To assume | To run away | I disagree | I disagree | I disagree | I disagree | ||||||
| Religion is important | |||||||||||||
| Yes | -- | -- | -- | -- | -- | -- | Ref. | Ref. | |||||
| No | -- | -- | -- | -- | -- | -- | 0.8[0.7-0.9] | 0.8[0.6-0.9] | |||||
| Professional category | |||||||||||||
| Nurse | -- | -- | -- | -- | Ref. | Ref. | -- | -- | |||||
| Physician | -- | -- | -- | -- | 1.2[1.1-1.3] | 1.2[1.1-1.3] | -- | -- | |||||
| Graduation time | |||||||||||||
| ≤ 10 years | Ref. | Ref. | Ref. | Ref. | -- | -- | Ref. | Ref. | |||||
| 11-15 years | 3.2[0.9-11.1] | 1.9[0.5-6.7] | 5.0[1.1-23.2] | 2.7[0.6-11.9] | -- | -- | 0.9[0.8-1.1] | 0.9[0.8-1.1] | |||||
| > 15 years | 0.8[0.2-2.7] | 0.6[0.1-2.0] | 1.0[0.2-5.2] | 2.1[0.4-11.3] | -- | -- | 0.8[0.8-1.0] | 0.9[0.7-1.2] | |||||
| Death was discussed in working life | |||||||||||||
| Yes | -- | -- | -- | -- | Ref. | Ref. | -- | -- | |||||
| No | -- | -- | -- | -- | 0.8[0.7-0.9] | 0.8[0.7-0.9] | -- | -- | |||||
| First personal experience with death | |||||||||||||
| Childhood | -- | -- | -- | -- | Ref. | Ref. | -- | -- | |||||
| Adolescence | -- | -- | -- | -- | 0.9[0.8-1.0] | 0.9[0.8-1.4] | -- | -- | |||||
| Adult age | -- | -- | -- | -- | 0.8[0.7-1.0] | 0.8[0.7-0.9] | -- | -- | |||||
| Number of ICUs where you work | |||||||||||||
| 1 | Ref. | Ref. | Ref. | Ref. | -- | -- | -- | -- | |||||
| ≥ 2 | 3.7[1.3-10.8] | 0.7[0.2-2.8] | 4.8[1.3-17.7] | 1.8[0.3-9.5] | -- | -- | -- | -- | |||||
OR: Odds ratio; 95%CI: 95% confidence interval; Ref.: Reference category; Dashes (--): Not significant. Only variables with p-value < 0.05 in at least one of the adjusted models were kept. * The following variables entered in the adjusted model 3: Graduation time, working in ICU, load-time in the ICU, and ICU quantity in that work; † The following variables entered in the adjusted model 4: The participants discussed the theme of death in professional life, professional category, time of the first personal experience with death, having a religion, and living with a companion; ‡ The following variables entered in the adjusted model 5: Time of the first personal experience with death and professional category.
DISCUSSION
This study is pioneering in analyzing elements associated with the perceptions/feelings of professional attitudes towards the death of an ICU patient, which was performed exclusively with health workers in a public hospital in Brazilian Legal Amazon. The death of ICU patients especially meant failure/guilt for physicians and pain for nurses, while they understood the death of POTP as rest/relief for sick people. The physicians e nurses' perceptions/feelings on the death of ICU patients were associated with the labor category, age of the first personal experience with death, and ICU specialty. The professional attitudes toward the death of ICU patients were associated with the graduation time, professional category, ICUs quantity on which works, death discussion during professional life, age of the first personal experience with loss, and religion.
PERCEPTIONS/FEELINGS FACING THE DEATH (MODELS 1 AND 2)
The death of an ICU patient meant failure or fault to 26.8% of health workers, while the death of a terminally ill patient represented pain for the professional in 13.7% of the situations. The loss of an ICU patient is also considered a failure in other studies, linked to a technicist practice18,41,42. Despite medical advances improving patient care at the end of life, strategies such as hospitalization and palliative care have only achieved a partial success. Health professionals and patients have difficulty in accepting death. Medical training focused on the use of hard technologies, with little appreciation of the physician-patient relationship, contributes to the maintenance of life at any cost2. The feeling of unpreparedness, when faced with the patient's death, has been a constant challenge20, requiring the reinterpretation of death and the role of medicine. Sometimes the death of a patient is considered "necessary", and is understood as an anticipated and expected event which generates tranquility and peace; therefore, a "good death"6,7,21. The loss of patients generates feelings such as frustration, helplessness, sadness, compassion, failure, pain, and others. It is common to use defensive strategies by health professionals, such as rationalization and distancing18,41,43.
In the specific context of the pediatric ICU, the meaning of death has different nuances7,20,21. For health professionals, these meanings are likely determined by previous experiences, personal beliefs, and the degree of emotional involvement with the person who died. However, it is known just a little about such determinants. Studies indicate that spirituality and religion are factors that potentially affect those concepts in different societies44,45,46. In the present study, although analyses of associations stratified by ICU specialty were not carried out, it was possible to identify that the perceptions/feelings of professionals regarding the death of a patient in a pediatric ICU did not differ from those of a general ICU, contrary to the expectative. A possible explanation is that the intensity of feelings was not measured, which was perhaps stronger in the face of the children death.
The following factors were associated with a higher chance of understanding death as a "failure or guilt" of professionals and not as "beginning/freedom" for the patient: i) having the first personal experience of death in adulthood, compared to childhood; ii) being a physician, compared to being a nurse; and iii) working in the cardiology ICU, compared to general ICU. Those who had worked longer in ICUs were more likely to understand death as an "ending" and not as a "beginning/freedom". These results are unprecedented in the literature and point to the need for participation in death rituals at an early age and more thematic discussion during medical training. Over half of the respondents revealed that their first personal contact with death occurred during childhood and adolescence; thus, the construction of beliefs related to loss occurred long before "professionalization". Early exposure appears to allow a certain familiarity with the "rites of passage" in different cultures.
In this study, only 49.5% of health workers discussed the death theme during graduation and 42.7% during postgraduation, so it can be noticed that discussing death and dying appears crucial in developing professional attitudes6,13,14,15,18,43,45. The development of skills in solving problems, communication with the patient and family, and emotional control are essential for providing such care47. Despite this, teaching communication and relationship techniques appears insufficient. Professionals must accept their vulnerability and be able to express themselves, as well as share their feelings without fear48.
The study results show that nurses were more likely to understand the death of POTP as a "painful" experience for themselves and not as "rest or relief" for the patient. Terminal illness brings great existential suffering22. Nurses may interpret the death of POTP as "pain" for themselves more often than physicians, because of their greater involvement in the patients' daily care.
The humanistic role model suggests that empathy is a decisive element in the care of a patient. Being empathetic allows one to develop the skills to treat patients who are dying18,22,49. When recognizing the meaning of death, the professional starts perceiving it, not just with horror and a sense of tragedy, but with responsibility for caring39.
PROFESSIONAL ATTITUDES FACED WITH THE DEATH OF AN ICU PATIENT (MODELS 3, 4, AND 5)
In this study, the professional attitudes of nurses and physicians when faced with the death of an ICU patient were mainly associated with professional training and religiosity. Professionals with longer training who had worked in a higher number of ICUs were more likely to take responsibility for communicating the news of death to the family, rather than sharing that responsibility with the multidisciplinary team.
Studies on the communication of bad news are scarce. In Basel, Switzerland, the interviews with 17 nurses and 14 physicians identified a desire to talk about death with patients at the end of life. However, obstacles were identified, such as a lack of time and privacy (45.2%), confrontation with their mortality (38.7%), resistance or denial (38.7%), and the poor cognitive status of the patient (22.6%). Moreover, the excessively long working hours of ICU workers may represent an obstacle to better doctor-patient interactions50. The adoption of bad news protocols has improved communication between professionals, patients, and families47.
In this investigation, physicians discussed death less than nurses, and those whose first professional experience of loss was with a child were more likely to argue for the resuscitation of POTP. Nursing students were better prepared to face the deaths compared to medicine students22. However, nursing students felt less ready to talk about the death of young children compared to medical students. These findings demonstrate the importance of a broader discussion in Brazilian society about the ethical issues involved in POTP, given the limited protocols and ethical references4,5,25.
For health students, the first contact with death is through a lifeless body in the anatomy room, i.e., in a distant, dehumanized way48. The training curriculum should include philosophical principles and professional attitudes faced with death13,45,51. The first discussions on the subject usually occur only during working life, after graduation, and postgraduation51, which can contribute to an attitude of indifference and detachment48. There are essential differences between physicians' and nurses' training, because the first focuses on technical improvement, and the second emphasizes on a comprehensive and holistic approach4,13,48. Topics such as the resuscitation of POTP and practices like euthanasia, dysthanasia, and orthothanasia are already widely discussed in some countries of the world, but not enough in Brazil2,7,12,20,27. The findings of the present study suggest the need for improvements in curricula for dealing with patients at the end of life in Brazil, similar to some other authors13,45,51.
Suspending intensive treatment is a difficult task in ICUs11. In the pediatric ICU, 41% of deaths were linked to decisions around the withdrawal/non-adoption of life support measures and, according to this, physicians and nurses do not feel confident about the decision to remove such care11,15,20,45,48. In a study conducted in Macedonia on 217 ICU physicians, most have little or no formal training (67%) in their academic life, highlighting the need to review undergraduate and graduate programs and the ongoing training of ICU professionals working with patients at the end of life51,52. ICUs should have protocols for dealing with such situations based on multidisciplinary decisions, not just the physicians' judgment. They must consider ethical aspects in this deliberation, along with the patient's and family's wishes5,53.
For this study, professionals who reported not giving central importance to religion were more likely to agree on the idea of discussing the resuscitation possibility with the patient's family. That is, they allowed the family to share this decision. A study conducted to analyze the influence of religion on medical decisions for terminally ill patients included 304 physicians, 386 nurses, 248 patients, and 330 family members of patients in 142 ICUs from six European countries44, divided into Protestant, Catholic, Jewish, or without religion. Religious people tended to require more prolongation of life and less euthanasia, and professionals suggested fewer invasive procedures than patients and their families. Seventy-five percent of physicians and nurses said they respected the patient's opinion. Protestants preferred to follow the patient's wishes, and Jews were more likely to authorize ineffective treatment44. Religion seems to be a decisive factor for health professionals in dealing with the death of ICU patients54. It is necessary to understand that religious and spiritual practices are integral and cultural elements of fundamental importance to the holistic health of their patients if healthcare professionals are to support patients and their families in end-of-life care45.
STUDY LIMITATIONS AND STRENGTHS
This study focuses on a relevant theme to the humanization of the end-of-life for ICU patients and the understanding of its determinants. Although we had searched a single hospital, this is a state reference facility and a teaching hospital, with large numbers of beds, and critical care professionals from different specialties, who generally work in some other ICU, contributing to increasing the representativeness of the sample. This diversity allows a more accurate diagnosis about the factors that affect the thoughts and professional attitudes of health workers when facing patients' death in ICU. Even so, due to the fact of being developed in only one center, we are not able to generalize our results, besides there is another limit related to the questionnaire validity and reliability. We just did the initial steps of the face and content validation with a team of experts, but we did not perform validation using more sophisticated statistical analysis, a strategy that was already reported by some other authors in health science53,55. Additionally, other limitations were: the impossibility of identifying all the feelings related to the death of ICU patients, as the professionals did not specifically answer what these other feelings were; and the relatively small sample size, which did not allow analyzes stratified by ICU specialty.
We used five different outcomes to assess the meaning of death, and the professional attitudes towards an ICU patient's death. These items are not able to widely determine the meaning of death and, especially, professional attitudes. However, we focused on some emblematic and impactful decisions in maintaining life and accepting death. The low rate of losses due to the non-return of their questionnaires (6.8%), the use of self-administered questionnaires, and the use of multivariate analysis with a hierarchical approach contributed to reducing the possibility of bias. Furthermore, in this study, we obtained a great adhesion of physicians, suggesting the relevance of the theme.
CONCLUSION
The death of ICUs patients is linked to feelings of pain, guilt, and failure for nurses and physicians in one Capital city of the Brazilian Legal Amazon. The professional attitudes revealed a strong therapeutic obstinacy. The professional perceptions/feelings and attitudes facing death are affected by sociocultural aspects, previous experience, and vocational training. From these findings, curriculum changes and the implementation of palliative care and bad news transmission protocols in the ICUs are suggested, as well as offering permanent education and psychological support to workers in this Brazilian strategic area. Some consequences of this investigation can already be seen: Professionals from the city's ICUs have systematically discussed the theme of death, re-signifying the loss of ICU patients, and re-adapting their practices. Undergraduate and postgraduate courses in the health area, such as Medicine and Nursing, in both public and private sectors, are incorporating courses on death in their curricular components.